Hemorrhoids Online Registration
 Every year, hundreds of thousands of people are diagnosed with colon or rectum cancer. While anorectal symptoms and complaints are common and typically not a serious concern, all patients should be examined for signs of possible cancer. Common symptoms of anorectal disease include rectal pain, bleeding, anal itching and a rectal mass or lump.
Every year, hundreds of thousands of people are diagnosed with colon or rectum cancer. While anorectal symptoms and complaints are common and typically not a serious concern, all patients should be examined for signs of possible cancer. Common symptoms of anorectal disease include rectal pain, bleeding, anal itching and a rectal mass or lump.
Patients should be checked for anorectal disease as early as possible if symptoms arise. If caught in its early stages, the cancer will require less extensive treatment and stress for the patient. Patient assessments must include an anorectal exam, flexible sigmoidoscopy, or a colonoscopy. For colorectal cancer, patients 50 years or older in the general population and 40 years or older with risk factors/family history of the disease should begin regular screenings.
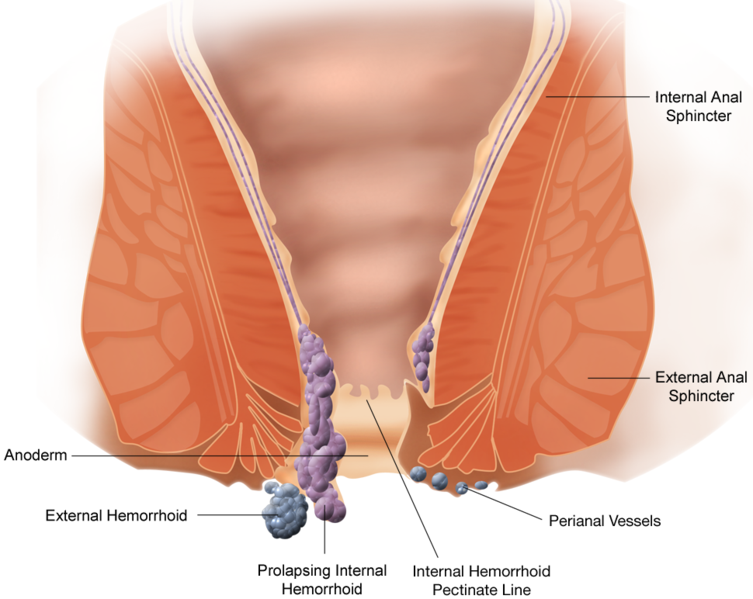
Anorectal Anatomy
The anus is the outlet to the gastrointestinal tract, while the rectum is the lower 10-15 centimeters of the large intestine. The dentate line divides the outer skin from the mucosa, the intestinal mucous membrane. The area of the rectum above the dentate line does not contain pain nerves, which allows for surgical procedures to be performed without anesthesia. However, the area below the dentate line is highly sensitive.
Four to eight anal glands drain into the crypts of Morgagni at the dentate line; most rectal abscesses and fistulae originate in these glands. Bowel movements are controlled by both the involuntary internal sphincter and the voluntary external sphincter muscles.
Anorectal Exam

During an inspection, the patient typically lies sideways on his or her left side, which allows more comfort as well as good visualization and access for the examiner. The doctor often locates external hemorrhoids, anal polyps, and anal fissures or fistulas using this method.
A digital exam is used to palpate (examine by touch) any suspicious mass lesions in the anorectal canal.
An anoscopy is used to confirm a diagnosis for hemorrhoids, anal fissures and other anorectal diseases.
Anorectal Complications
Anal Itching

Treatments for anal itching include taking antihistamine as a sedative prior to sleeping to prevent unconscious scratching, or using a topical corticosteroid to alleviate the itching. Underlying disorders such as hemorrhoids must also be considered and treated when diagnosing and treating anal itching.
Anal Pain
 Anal pain is a common sign of anorectal disease. Pain caused by an acute anal fissure may occur during intense, forced bowel movements that are often accompanied by rectal bleeding.
Anal pain is a common sign of anorectal disease. Pain caused by an acute anal fissure may occur during intense, forced bowel movements that are often accompanied by rectal bleeding.
Pain that begins gradually and becomes excruciating may indicate infection, while a fever and inability to urinate indicates need for emergency treatment.
Immediate onsets of intense pain accompanied by a palpable mass are usually caused by an external thrombosed hemorrhoid, which can last a few days to a couple of weeks. Internal hemorrhoids, however, are not painful due to being located above the dentate line of the rectum, where there are no pain nerves. Similarly, rectal cancer typically does not cause pain unless the condition is advanced. Patients with chronic anal fissures usually have intermittent sharp rectal pain and bleeding with each bowel movement for an extended period of time.
Proctalgia fugax is a more serious anal pain condition that involves short spasms of intense pain at night. This condition can occur anywhere from once per year up to 3-4 times each week. The pain is typically accompanied by sweating and an urge to pass stool. There is currently no treatment for proctalgia fugax, but placing oneself in hot water or applying ice may provide symptomatic relief.
Rectal Lumps

- Hemorrhoids are probably the most common reason for having a rectal lump. If related to internal hemorrhoids, the lump usually enlarges and becomes more prolapsed after a bowel movement. It can usually be spontaneously reduced in its early stages and is often associated with other symptoms such as bleeding, itching or pain. Thrombosed external hemorrhoids, however, are usually very painful.
- Anal warts are caused by the human papilloma virus (HPV), considered a sexually transmitted diseases. If left untreated, anal warts can spread and increase the risk of cancer in the anorectal region.
- An anal fissure is a small cut or split in the anal lining often caused by a painful, forced bowel movement. Fissures are typically located anterior or posterior to the anus. They’re often associated with a lump called a sentinel pile, accompanied by pain and bleeding.
- Anal cancer occurs in the anal canal and accounts for roughly two percent of cancers in the gastrointestinal tract. The cancer can take several forms including ulcers, polyps or verrucous growths. An external or internal mass may be palpable, but anal or rectal cancer generally doesn’t produce any pain. Some lesions can be so soft that they’re missed on palpation.
Rectal Bleeding
Rectal bleeding refers to the passage of red blood from the rectum and anus, often mixed with stool and/or blood clots. The severity of rectal bleeding varies widely, ranging from mild/intermittent to moderate or severe.
Rectal bleeding can be caused by various conditions, but even the slightest amount of bleeding should be taken seriously. Common causes of bleeding are internal hemorrhoids, ruptured thrombosed external hemorrhoids, fissures, diverticulosis, colon cancer, colitis, polyps and angiodysplasias. Patients of older age or with significant family history of bowel disease or cancer should consider further examination. Patients who were previously treated for rectal bleeding but continue to experience bleeding must be further examined.
The source of one’s rectal bleeding is determined by medical history and a physical examination using blood tests, an anoscopy, sigmoidoscopy, colonoscopy, radionuclide scans, and angiograms.