The Story of St. Fiacre, Patron Saint of Hemorrhoid Sufferers
Did Bad Hemorrhoids Cause Napoleon to Lose at Waterloo?
Hemorrhoid Treatment on the Road
The Treatment of Hemorrhoids in Ancient and Modern Times
Major Moments in Hemorrhoids History
The Story of St. Fiacre, Patron Saint of Hemorrhoid Sufferers
 More than 10 million people in the United States suffer from hemorrhoids. Three out of four people in Minnesota will develop hemorrhoids at some point in their lives. In fact, the disease is so common that hemorrhoid sufferers have their own patron saint, St. Fiacre.
More than 10 million people in the United States suffer from hemorrhoids. Three out of four people in Minnesota will develop hemorrhoids at some point in their lives. In fact, the disease is so common that hemorrhoid sufferers have their own patron saint, St. Fiacre.
During the middle ages, an integral part of treating certain ailments involved praying to patron saints in hopes of divine intervention. Based on legends surrounding his life, St. Fiacre, a 7th century Irish monk, became the patron saint for hemorrhoid sufferers, and hemorrhoids were known as St. Fiacre’s curse. St. Fiacre was also deemed the patron saint of gardeners due to his ability to successfully farm and cultivate all the land in a single day. As the legend goes, the saint was given a small shovel by his bishop and spent long days tirelessly spading his garden before soon developing a severe case of prolapsed hemorrhoids. Seeking a solution, St. Fiacre sat on a stone and prayed for help. His prayers were later answered in the form of a miracle.
Source: St. Fiacre: Patron Saint of Hemorrhoid Sufferers
Did Bad Hemorrhoids Cause Napoleon to Lose at Waterloo?
 A theory that has been passed down throughout history states that Napoleon had suffered an extreme case of hemorrhoids when the Battle of Waterloo went down, delaying his opening assault on the morning of June 18, 1815. The ever popular theory was actually detailed in the book, Napoleon’s Hemorrhoids: And Other Small Events That Changed History.
A theory that has been passed down throughout history states that Napoleon had suffered an extreme case of hemorrhoids when the Battle of Waterloo went down, delaying his opening assault on the morning of June 18, 1815. The ever popular theory was actually detailed in the book, Napoleon’s Hemorrhoids: And Other Small Events That Changed History.
It’s believed that Napoleon was unable to mount his horse on the final day of the battle, while also being accidentally overdosed with laudanum by his doctors. Failing to begin his attack on time, Napoleon allowed the Duke of Wellington enough time to join forces with Blucher.
However, Andrew Roberts, author of Napoleon & Wellington, and Waterloo expert Alisdair White both refute this theory.
Roberts stated that Napoleon had indeed suffered from hemorrhoids, which “had prolapsed and were strangulated outside the anus,” causing him great pain. Inflamed hemorrhoids, however, couldn’t have caused the military leader’s failure to attack Wellington that morning, as Napoleon was dressed and in saddle by 8 o’clock.
Roberts added that bad hemorrhoids and other medical conditions known to have afflicted Napoleon—cystitis, exhaustion, and constipation—were excuses employed by Napoleon apologists as a method to sustain the Corsican’s myth of invulnerability.
Source: Did Bad Hemorrhoids Cause Napoleon to Lose at Waterloo?
Hemorrhoid Treatment on the Road
 I have an interesting story from when I visited China many years ago. I was invited to give a lecture on office procedures as a guest professor at Zhejiang University. After the academic exchange, I had a few days to myself, so I went to visit an old friend of mine—let’s call him Dave.
I have an interesting story from when I visited China many years ago. I was invited to give a lecture on office procedures as a guest professor at Zhejiang University. After the academic exchange, I had a few days to myself, so I went to visit an old friend of mine—let’s call him Dave.
Dave and I decided to go visit a new resort town a few hours away from the city. As we were talking in the hotel, he began looking a bit shifty on the couch, as if he were very uncomfortable. After he spent an extended amount of time in the bathroom, I asked him if he was alright, to which he admitted that he was suffering from painful hemorrhoids. Thankfully, I was able to diagnose him with having a thrombosed hemorrhoid that needed immediate treatment. When a hemorrhoid clots, it develops localized bulging and becomes extremely painful, especially when going to the bathroom.
Dave said that he would go to the hospital, but he hesitated because of China’s inconvenient medical care. He didn’t trust the doctors working at the local hospital, and he was indecisive in choosing a larger hospital. I told him that I had fixed countless thrombosed hemorrhoids throughout my career, and that if I had the tools I needed, I could fix it for him in a flash. I went to a local hospital in town and identified myself as a general surgeon who attended Shanghai Medical University 20 years ago and who currently practices in the US. I asked if I could get the necessary gear to do the procedure. Amazingly, the staff were very helpful and generous, and I managed to return with latex gloves, a scalpel, syringes, a pack of gauze, and a bottle of Lidocaine. We were able to perform the procedure right there in the hotel.
The entire procedure only took a few minutes. I used 0.5 cc of Lidociaine to numb the top of the thrombosed hemorrhoid before slicing it open with a scalpel and removing the clotted blood with a cotton-tipped applicator. Once the clot was gone, I cleaned up the area by packing large amounts of gauze. The relief was immediate, and other than a little bleeding for a day or so, the problem was alleviated. I told Dave that if he ever gets the chance to visit Minneapolis, I could do IRC treatments to fix the root of his problem: internal hemorrhoids.
The Treatment of Hemorrhoids in Ancient and Modern Times
 Hemorrhoids, a condition that involves swelling of the veins in the rectum, have been a nuisance since the dawn of man. Accounts of hemorrhoids date back to the earliest of civilizations, including the Egyptians, the Greeks and the Romans.
Hemorrhoids, a condition that involves swelling of the veins in the rectum, have been a nuisance since the dawn of man. Accounts of hemorrhoids date back to the earliest of civilizations, including the Egyptians, the Greeks and the Romans.
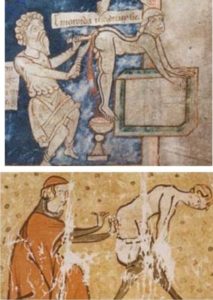
Ancient Egyptian documents directed caregivers to apply an ointment made from ground acacia tree for an unnamed, but painful, perianal disease that was most likely hemorrhoids. The word “haemorrhoid” has Greek roots: haema (blood) and rhoos, coined by Hippocrates in 460 BC. Hippocrates provided some of the earliest recorded methods of surgical procedures, including a ligation procedure that involved tying thick woolen thread around the hemorrhoid to cut off its blood supply. Later writings also described excision of hemorrhoids. The Roman, Arab and Indian societies also recorded writings that described their own ligation and excision techniques.
During the Middle Ages, these procedures were often performed by literal barber instead of physicians, who thought themselves to be above performing surgery. Barbers often had various tools essential to their trade that doubled as makeshift surgical equipment. Science and surgery met once again the during The Renaissance, where documents indicated the usage of ligation with needle and thread, followed by excision.
Clearly, ligation was the preferred way of operating on hemorrhoids. It was simple to do and only required readily available material. Even today, ligation is an incredibly common procedure offered by many clinics, including One Stop. Rubber band ligation, the modern version of the procedure, is not far off from that of ancient times. The procedure involves inserting an anoscope into the anus, grasping the hemorrhoid, then attaching a rubber band tightly around the base of the hemorrhoid. The hemorrhoid then shrivels up and falls off in about a week.
Nowadays, ligation is just one of multiple options and is performed depending on how advanced the hemorrhoids are. Infrared Coagulation Therapy, or IRC, is a procedure that has gained popularity for small to medium sized hemorrhoids. The device is inserted through an anoscope and will then apply infrared light directly to the hemorrhoid, which causes clotting and scar tissue. Scarring causes the hemorrhoid to shrink. Rubber band ligation is slightly more painful, but IRC has slightly higher chances of relapse. Ultimately, they are similar in effectiveness.
Major Moments in Hemorrhoids History
 Hemorrhoids have been an issue for people for as long as people have existed, and it’s fascinating to see its presence so universally throughout history. Remember- everyone gets hemorrhoids. Don’t be afraid to have them checked out by your doctor.
Hemorrhoids have been an issue for people for as long as people have existed, and it’s fascinating to see its presence so universally throughout history. Remember- everyone gets hemorrhoids. Don’t be afraid to have them checked out by your doctor.
Hemorrhoids have plagued humans for thousands of years, with the earliest known mention of its symptoms dating back to roughly ~2250 BC in the kingdom of Babylon in the Code of King Hammurabi. Fast forward to 1700 BC in Egypt, and we stumble upon the first-ever recorded case of hemorrhoids, which also happened to highlight an important topical wound ointment.
The first use of the word “haemorrhoids” in the English language occurred in 1398. The term derived from the Old French word “emorroides,” taken from Latin derivative “hæmorrhoida-ae,” which in turn originated from the Greek word for “haimorrhois.”
Below is a timeline of key events in the history of hemorrhoid development:
~2250 BC: Babylon Code of King Hammurabi described the symptoms of hemorrhoids
1700 BC: Egyptian papyrus pronounced a topical astringent lotion
1552 BC: Egyptian medical record detailed remedies for hemorrhoids
1046 BC: Old Testament, 1 Samuel 5:9 Philistines punished with “emerods”, and in 1 Samuel 5:12 People who moved the Ark to Ekron were punished with “emerods”
460–375 BC: Hippocratic Treatises described hemorrhoid treatment by cautery and excision, and first recorded use of speculum to inspect the rectum (endoscopy)
25 BC–AD 50: Celsus describes Pile ligation
41–68: Roman physician Dioscorides defined Aloe Vera use for easing hemorrhoids
130–200: Roman Emperor Marcus Aurelius’s physician Galen pronounced hemorrhoids treatment ointment containing laxatives and leeches. He also explained thread use to tie off piles causing them to shrivel up
4th–5th Century: Indian Susruta Samhita text defined clamp and cautery use
5th–10th Century: Arab physician El-Zahrawy defined cautery irons use, whilst Byzantine physicians ligated with thread on the hemorrhoid base, before amputating
1307–1370: John of Ardene’s exposition transcribed hemorrhoids and fistula treatment, and enemas use
1806: Modern era of endoscopy was piloted by Bozzini with his aluminum tube to expose the genitourinary tract
1835: St.Marks Hospital London was founded by Frederick Salmon providing modern hemorrhoids and fistula treatment
1849: Introduction of anal dilation for hemorrhoids treatment
1935: St.Marks Hospital further developed excision and ligation methods at the hands of ETC Milligan and C Naughton Morgan – nowadays defined as the gold inhemorrhoidectomy standard
1952: Modification to the Milligan-Morgan procedure introduced by Ferguson
1955: A.G. Parks’ developed his closed method surgical treatment the hemorrhoidectomy
1963: J Barron developed an out-patient rubber band procedure to tie hemorrhoids
1970: Development of cryotheraphy, diathermy, infrared coagulation and laser cauteries
1975: PH Lord developed his anal dilation hemorrhoid treatment method, whilst WHF Thompson postulated that hemorrhoids developed from anal cushions that are part of the normal anatomical structures
1997: Italian A Longo introduced his stapled hemorrhoidectomy procedure for prolapsed hemorrhoids
Due to lack of studies and documentation on hemorrhoids, as well as lack of patients seeking medical assistance, the exact prevalence of hemorrhoids is unknown. However, it’s estimated that roughly half of Americans develop hemorrhoids by age 50, with roughly five percent of the US population affected.
The outlook for hemorrhoid treatment and rehabilitation is generally positive. While some individuals suffer from flare-ups and recurring hemorrhoids, only a small portion of patients require surgery.
